Nurs 693 week 3 discussion Paper.
On completion of this chapter, the reader will be able to:
• Explain the purpose and components of the Apgar score.
• Describe how to perform a physical assessment of a newborn.
• Describe how to perform a gestational age assessment of a newborn. Nurs 693 week 3 discussion Paper.
• Compare the characteristics of the preterm, late preterm, term, and postterm neonate.
• Provide nursing care to assist the newborn to transition to extrauterine life.
ORDER A PLAGIARISM-FREE PAPER HERE.
• Explain the elements of a safe environment. Nurs 693 week 3 discussion Paper.
• Discuss phototherapy and the guidelines for teaching parents about this treatment.
• Explain the purposes and methods for circumcision, the postoperative care of the circumcised infant, and parent teaching regarding circumcision.
• Review the procedures for administering an intramuscular injection, performing a heelstick, collecting urine specimens, and venipuncture.
• Evaluate pain in the newborn based on physiologic changes and behavioral observations.
• Review anticipatory guidance nurses provide to parents before discharge.
Although most infants make the necessary biopsychosocial adjustments to extrauterine existence without undue difficulty, their well-being depends on the care they receive from others. This chapter describes the assessment and care of the infant immediately after birth until discharge, as well as important anticipatory guidance related to ongoing infant care. A discussion of pain in the neonate and its management is included.
Care Management: Birth Through the First 2 Hours
Care begins immediately after birth and focuses on assessing and stabilizing the newborn’s condition. The nurse has the primary responsibility for the infant during this period because the physician or nurse midwife is involved with care of the mother. The nurse must be alert for any signs of distress and initiate appropriate interventions. Nurs 693 week 3 discussion Paper.
With the possibility of transmission of viruses such as hepatitis B virus (HBV) and human immunodeficiency virus (HIV) through maternal blood and blood-stained amniotic fluid, the newborn must be considered a potential contamination source until proved otherwise. As part of Standard Precautions, nurses wear gloves when handling the newborn until blood and amniotic fluid are removed by bathing. Nurs 693 week 3 discussion Paper.
The foundation for providing comprehensive, family-centered newborn care is awareness of the mother’s preconception and prenatal history as well as intrapartal events. Recognition of risk factors (Box 23-1) enables the nurse to be more astute in observations and assessments and more likely to identify early signs of complications. This allows for earlier intervention and promotes positive outcomes.
Immediate Care After Birth
The primary goal of care in the first moments after birth is to assist the newly born infant to transition to extrauterine life by establishing effective respirations. If the infant is at term, is crying or breathing, and has good muscle tone, routine care can begin (Kattwinkel, Perlman, Aziz, et al., 2010). Nurs 693 week 3 discussion Paper. The infant is placed prone on the mother’s abdomen or chest, and the nurse assesses the airway. Slight extension of the neck helps keep the airway patent. Drying the infant with vigorous rubbing removes moisture to prevent evaporative heat loss and provides tactile stimulation to stimulate respiratory effort. The mother and her newborn are covered with a warm blanket (Niermeyer and Clarke, 2011).
If the neonate is apneic or has gasping respirations, positive-pressure ventilation is needed. The heart rate is quickly assessed by grasping the base of the cord or by auscultating the left chest with a stethoscope. Count for 6 seconds and multiply by 10 to calculate the heart rate. It should be greater than 100 beats/min. The newborn’s trunk and lips should be pink; acrocyanosis is a normal finding (see Fig. 22-4) (Niermeyer and Clarke, 2011).
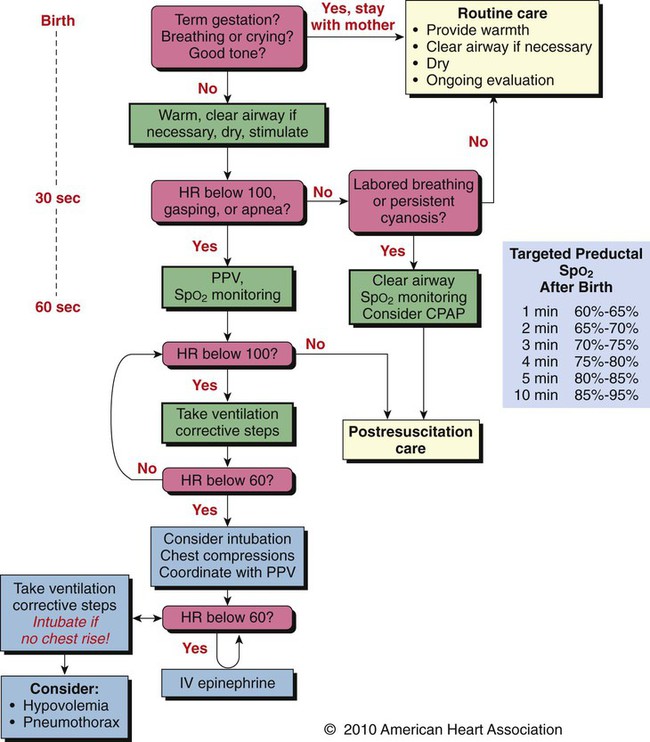
If the newborn requires respiratory or circulatory support, the nurse and other members of the health care team (e.g., neonatologist, respiratory therapist) follow the American Heart Association guidelines for neonatal resuscitation (Kattwinkel, Perlman, Aziz, et al., 2010). The neonatal resuscitation algorithm directs the care (Fig. 23-1).
As soon as possible after birth, the nurse places identically numbered bands on the infant’s wrist and ankle, on the mother, and on the father or significant other. An electronic infant security tag or abduction system alarm should be placed on all newborns to aid in protecting against infant abduction. The infant is footprinted with ink or a scanning device within 2 hours of birth (Vincent, 2009). (See later discussion of infant abduction.)
Apgar Scoring and Initial Assessment
The initial assessment of the neonate is performed immediately after birth using the Apgar score (Table 23-1) and a brief physical examination (Table 23-2). A gestational age assessment is completed within the first hours of birth in a stable newborn (Fig. 23-2). A more comprehensive physical assessment is completed within 24 hours of birth (Table 23-3).
TABLE 23-1
| SIGN | SCORE | ||
| 0 | 1 | 2 | |
| Heart rate | Absent | Slow (<100/min) | >100/min |
| Respiratory effort | Absent | Slow, weak cry | Good cry |
| Muscle tone | Flaccid | Some flexion of extremities | Well flexed |
| Reflex irritability | No response | Grimace | Cry |
| Color | Blue, pale | Body pink, extremities blue | Completely pink |
TABLE 23-2
INITIAL PHYSICAL ASSESSMENT OF THE NEWBORN
| General appearance |  Color pink Color pink |
|
 Acrocyanosis present Acrocyanosis present |
||
 Flexed posture Flexed posture |
||
 Alert Alert |
||
 Active Active |
||
| Respiratory system |  Airway patent Airway patent |
|
 No upper airway congestion No upper airway congestion |
||
 No retractions or nasal flaring No retractions or nasal flaring |
||
 Respiratory rate, 30-60 breaths/min Respiratory rate, 30-60 breaths/min |
||
 Lungs clear to auscultation bilaterally Lungs clear to auscultation bilaterally |
||
 Chest expansion symmetric Chest expansion symmetric |
||
| Cardiovascular system |  Heart rate strong and regular Heart rate strong and regular |
|
 No murmurs heard No murmurs heard |
||
 Pulses strong and equal bilaterally Pulses strong and equal bilaterally |
||
| Neurologic system |  Moves extremities Moves extremities |
|
 Normotonic Normotonic |
||
 Symmetric features, movement Symmetric features, movement |
||
 Reflexes present: Reflexes present: |
||
 Sucking Sucking |
 Rooting Rooting |
|
 Moro Moro |
 Grasp Grasp |
|
 Anterior fontanel soft and flat Anterior fontanel soft and flat |
||
| Gastrointestinal system |  Abdomen soft, no distention Abdomen soft, no distention |
|
 Cord attached and clamped Cord attached and clamped |
||
 Anus appears patent Anus appears patent |
||
| Eyes, nose, mouth |  Eyes clear Eyes clear |
|
 Palates intact Palates intact |
||
 Nares patent Nares patent |
||
| Skin |  No signs of birth trauma No signs of birth trauma |
|
 No lesions or abrasions No lesions or abrasions |
||
| Genitourinary system |  Normal genitalia Normal genitalia |
|
| Other |  No obvious anomalies No obvious anomalies |
|
| Comments:_________________________________________________________________________________________________________________________________________________________ | ||
TABLE 23-3
PHYSICAL ASSESSMENT OF THE NEWBORN
| AREA ASSESSED AND APPRAISAL PROCEDURE | NORMAL FINDINGS | DEVIATIONS FROM NORMAL RANGE: POSSIBLE PROBLEMS (ETIOLOGY) | |
| AVERAGE FINDINGS | NORMAL VARIATIONS | ||
| Posture | |||
| Inspect newborn before disturbing for assessmentRefer to maternal chart for fetal presentation, position, and type of birth (vaginal, surgical), given that newborn readily assumes in utero position | Vertex: arms, legs in moderate flexion; fists clenchedResistance to having extremities extended for examination or measurement, crying possible when attemptedCessation of crying when allowed to resume curled-up fetal position (lateral)Normal spontaneous movement bilaterally asynchronous (legs moving in bicycle fashion) but equal extension in all extremities | Frank breech: legs straighter and stiff, newborn assuming intrauterine position in repose for a few daysPrenatal pressure on limb or shoulder possibly causing temporary facial asymmetry or resistance to extension of extremities | Hypotonia, relaxed posture while awake (preterm or hypoxia in utero, maternal medications, neuromuscular disorder such as spinal muscular atrophy)Hypertonia (chemical dependence, central nervous system [CNS] disorder)Limitation of motion in any of extremities |
| Vital Signs | |||
| Check heart rate and pulses: | |||
| Thorax (chest) | |||
| Inspection | Visible pulsations in left midclavicular line, fifth intercostal space | ||
| Palpation | Apical pulse, fourth intercostal space 120-160 beats/min when awake | 80-100 beats/min (sleeping) to 180 beats/min (crying); possibly irregular for brief periods, especially after crying | Tachycardia: persistent, ≥180 beats/min (respiratory distress syndrome [RDS]; pneumonia)Bradycardia: persistent, ≤80 beats/min (congenital heart block, maternal lupus) |
| Quality: first sound (closure of mitral and tricuspid valves) and second sound (closure of aortic and pulmonic valves) sharp and clear | Murmur, especially over base or at left sternal border in interspace 3 or 4 (foramen ovale anatomically closing at approximately 1 yr) | Murmur (possibly functional)Dysrhythmias: irregular rateSounds:
Heart on right side of chest (dextrocardia, often accompanied by reversal of intestines) |
|
| Peripheral pulses: femoral, brachial, popliteal, posterior tibial | Peripheral pulses equal and strong | Weak or absent peripheral pulses (decreased cardiac output, thrombus, possible coarctation of aorta if weak on left and strong on right)Bounding | |
| Obtain temperature: | |||
| Axillary: method of choiceTemporal and intraauricular thermometers not effective in measuring newborn temperature | Axillary: 37° C (98.6° F)Temperature stabilized by 8-10 hr of age | 36.5°-37.5° C (97.7°-100° F)Heat loss: from evaporation, conduction, convection, radiation | Subnormal (preterm birth, infection, low environmental temperature, inadequate clothing, dehydration)Increased (infection, high environmental temperature, excessive clothing, proximity to heating unit or in direct sunshine, chemical dependence, diarrhea and dehydration)Temperature not stabilized by 6-8 hr after birth (if mother received magnesium sulfate, newborn less able to conserve heat by vasoconstriction; maternal analgesics possibly reducing thermal stability in newborn) |
| Observe and monitor respiratory rate and effort: | |||
| Observe respirations when infant is at restObserve respiratory effortCount respirations for full minuteAuscultate breath soundsListen for sounds audible without stethoscope | 40/minTendency to be shallow and irregular in rate, rhythm, and depth when infant is awakeCrackles may be heard after birthNo adventitious sounds audible on inspiration and expirationBreath sounds: bronchial; loud, clear | 30-60/minShort periodic breathing episodes and no evidence of respiratory distress or apnea (>20 sec); periodic breathingFirst period (reactivity): 50-60/minSecond period: 50-70/minStabilization (1-2 days): 30-40/minCrackles (fine) | Apneic episodes: >20 sec (preterm infant: rapid warming or cooling of infant; CNS or blood glucose instability)Bradypnea: <25/min (maternal narcosis from analgesics or anesthetics, birth trauma)Tachypnea: >60/min (RDS, transient tachypnea of the newborn, congenital diaphragmatic hernia)Breath sounds:
Distress evidenced by nasal flaring, grunting, retractions, labored breathingStridor (upper airway occlusion) |
| Obtain blood pressure (BP) (usually not done in normal term infant) | |||
| Check oscillometric monitor BP cuff: BP cuff width affects readings, use appropriate-size cuff and palpate brachial, popliteal, or posterior tibial pulse (depending on measurement site) | 60-80/40-50 mm Hg (approximate ranges)At birth
At 2 weeks |
Variation with change in activity level: awake, crying, sleeping | Difference between upper and lower extremity pressures (coarctation of aorta)Hypotension (sepsis, hypovolemia)Hypertension (coarctation of aorta, renal involvement, thrombus) |
| Weight | |||
| Put cloth or paper protective liner in place and adjust scale to 0 g or pounds and ouncesWeigh at same time each dayProtect newborn from heat loss | Female: 3400 g (7.5 lb)Male: 3500 g (7.7 lb)Regaining of birth weight within first 2 weeks. Nurs 693 week 3 discussion Paper. | 2500-4000 g (5.5-8.8 lb)Acceptable weight loss: 10% or less in first 3-5 daysSecond baby weighing more than first (on average) | Weight ≤2500 g (preterm, small for gestational age, rubella syndrome)Weight ≥4000 g (large for gestational age, maternal diabetes, heredity—normal for these parents)Weight loss more than 10% to 15% (growth failure, dehydration); assess breastfeeding success |
 |
|||
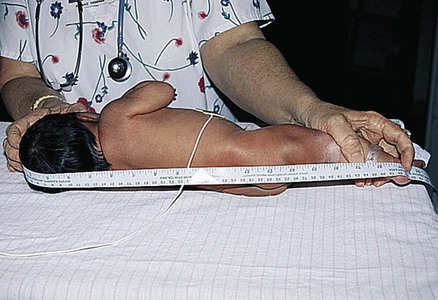
| Length | |||
| Measure length from top of head to heel; measuring is difficult in term infant because of presence of molding, incomplete extension of knees | 50 cm (19.7 in) | 45-55 cm (17.7-21.7 in) | <45 cm (17.7 in) or >55 cm (21.7 in) (chromosomal abnormality, heredity—normal for these parents); some syndromes present shorter-than-average limb length (skeletal dysplasias, achondroplasia) |
 ORDER A PLAGIARISM-FREE PAPER HERE. |
|||
| Head Circumference | |||
| Measure head at greatest diameter: occipitofrontal circumferenceMay need to remeasure on second or third day after resolution of molding and caput succedaneum | 33-35 cm (13-13.8 in)Circumference of head and chest approximately the same for first 1 or 2 days after birth; chest rarely measured on routine basis | 32-36.8 cm (12.6-14.5 in) | Microcephaly, head ≤32 cm: (maternal rubella, toxoplasmosis, cytomegalovirus, fused cranial sutures [craniosynostosis])Hydrocephaly: sutures widely separated, circumference ≥4 cm more than chest circumference (infection)Increased intracranial pressure (hemorrhage, space-occupying lesion) |
| Chest Circumference | |||
| Measure at nipple line | 2-3 cm (0.8-1.2 in) less than head circumference; average 30-33 cm (11.8-13 in) | ≤30 cm | Prematurity |
| Skin | |||
| Check color: | Generally pinkVaries with ethnic origin, skin pigmentation beginning to deepen right after birth in basal layer of epidermisAcrocyanosis common after birth. Nurs 693 week 3 discussion Paper. | MottlingHarlequin signPlethoraTelangiectases (“stork bites” or capillary hemangiomas) (see Fig. 22-6, A)Erythema toxicum/neonatorum (“newborn rash”) (see Fig. 22-6, B)MiliaPetechiae over presenting partEcchymoses from forceps in vertex births or over buttocks, genitalia, and legs in breech births | Dark red (preterm, polycythemia)Gray (hypotension, poor perfusion)Pallor (cardiovascular problem, CNS damage, blood dyscrasia, blood loss, twin-to-twin transfusion, infection)Cyanosis (hypothermia, infection, hypoglycemia, cardiopulmonary diseases, neurologic or respiratory malformations)Generalized petechiae (clotting factor deficiency, infection)Generalized ecchymoses (hemorrhagic disease) |
| Observe for jaundice | None at birth | Physiologic jaundice in up to 60% of term infants in first week of life | Jaundice within first 24 hr (increased hemolysis, Rh isoimmunization, ABO incompatibility) |
| Observe for birthmarks or bruises: | Mongolian spot (see Fig. 22-5) in infants of African-American, Asian, and Native-American origin | HemangiomasNevus flammeus: port-wine stainNevus vasculosus: strawberry markCavernous hemangioma | |
| Check skin condition: | Edema confined to eyelid (result of eye prophylaxis)Opacity: few large blood vessels visible indistinctly over abdomen | Possibly puffy Slightly thick; superficial cracking, peeling, especially of hands, feetNo visible blood vessels, a few large vessels clearly visible over abdomen.Some fingernail scratches | Edema on hands, feet; pitting over tibia; periorbital (overhydration; hydrops)Texture thin, smooth, or of medium thickness; rash or superficial peeling visible (preterm, postterm)Numerous vessels very visible over abdomen (preterm)Texture thick, parchment-like; cracking, peeling (postterm)Skin tags, webbingPapules, pustules, vesicles, ulcers, maceration (impetigo, candidiasis, herpes, diaper rash) |
| Weigh infant routinely | Dehydration: loss of weight best indicator | Normal weight loss after birth: up to 10% of birth weight | |
| Gently pinch skin between thumb and forefinger over abdomen and inner thigh to check for turgor | After pinch released, skin returns to original state immediately | Loose, wrinkled skin (prematurity, postmaturity, dehydration: fold of skin persisting after release of pinch)Tense, tight, shiny skin (edema, extreme cold, shock, infection) | |
| Note presence of subcutaneous fat deposits (adipose pads) over cheeks, buttocks | Variation in amount of subcutaneous fat | Lack of subcutaneous fat, prominence of clavicle or ribs (preterm, malnutrition) | |
| Check for vernix caseosa: | Whitish, cheesy, odorless | Usually more found in creases, folds | Absent or minimal (postmature infant)Abundant (preterm)Green color (possible in utero release of meconium or presence of bilirubin)Odor (possible intrauterine infection) |
| Assess lanugo: | Over shoulders, pinnas of ears, forehead | Variation in amount | Absent (postmature)Abundant (preterm, especially if lanugo abundant, long, and thick over back) |
| Head | |||
| Palpate skin | (See “Skin”) | Caput succedaneum, possibly showing some ecchymosis (see Fig. 22-10, A) | Cephalhematoma (see Fig. 22-10, B) |
| Inspect shape, size | Making up one fourth of body lengthMolding (see Fig. 22-9) | Slight asymmetry from intrauterine positionLack of molding (preterm, breech presentation, cesarean birth) | Severe molding (birth trauma)Indentation (fracture from trauma) |
| Palpate, inspect, and note size and status of fontanels (open vs. closed) | Anterior fontanel 5-cm diamond, increasing as molding resolves Posterior fontanel triangle, smaller than anterior | Variation in fontanel size with degree of molding Difficulty in feeling fontanels possible because of molding | Fontanels: |
| Palpate sutures | Palpable and separated sutures | Possible overlap of sutures with molding | Sutures: |
| Inspect pattern, distribution, amount of hair; feel texture | Silky, single strands lying flat; growth pattern toward face and neck | Variation in amount | Fine, wooly (preterm)Unusual swirls, patterns, or hairline; or coarse, brittle (endocrine or genetic disorders) |
| Eyes | |||
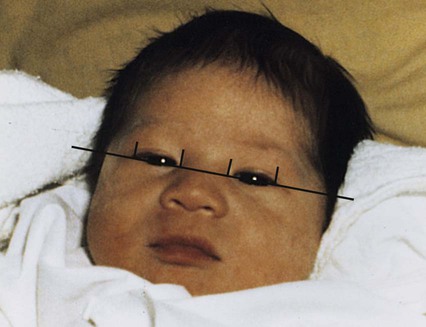
| Check placement on face | Eyes and space between eyes each one-third the distance from outer-to-outer canthus | Epicanthal folds: characteristic in some ethnicities | Epicanthal folds when present with other signs (chromosomal disorders such as Down, cri-du-chat syndromes) |
| Check for symmetry in size, shape | Symmetric in size, shape | ||
| Check eyelids for size, movement, blink | Blink reflex | Edema if eye prophylaxis drops or ointment instilled | |
| Assess for discharge | NoneNo tears | Some discharge if silver nitrate usedOccasional presence of some tears | Discharge: purulent (infection)Chemical conjunctivitis from eye medication is common—requires no treatment |
| Evaluate eyeballs for presence, size, shape | Both present and of equal size, both round, firm | Subconjunctival hemorrhage | Agenesis or absence of one or both eyeballsLens opacity or absence of red reflex (congenital cataracts, possibly from rubella, retinoblastoma [cat’s eye reflex])Lesions: coloboma, absence of part of iris (congenital)Pink color of iris (albinism)Jaundiced sclera (hyperbilirubinemia) |
| Check pupils | Present, equal in size, reactive to light | Pupils: unequal, constricted, dilated, fixed (intracranial pressure, medications, tumor) | |
| Evaluate eyeball movement | Random, jerky, uneven, focus possible briefly, following to midline | Transient strabismus or nystagmus until third or fourth month | Persistent strabismusDoll’s eyes (increased intracranial pressure)Sunset (increased intracranial pressure) |
| Assess eyebrows: amount of hair, pattern | Distinct (not connected in midline) | Connection in midline (Cornelia de Lange syndrome) | |
| Nose | |||
| Observe shape, placement, patency, configuration | MidlineSome mucus but no drainagePreferential nose breatherSneezing to clear nose | Slight deformity (flat or deviated to one side) from passage through birth canal | Copious drainage (rarely congenital syphilis); blockage membranous or bone with cyanosis at rest and return of pink color with crying (choanal atresia)Malformed (congenital syphilis, chromosomal disorder)Flaring of nares (respiratory distress) |
| Ears | |||
| Observe size, placement on head, amount of cartilage, open auditory canal | Correct placement line drawn through inner and outer canthi of eyes reaching to top notch of ears (at junction with scalp)Well-formed, firm cartilage | Size: small, large, floppy Darwin’s tubercle (nodule on posterior helix)
Nurs 693 week 3 discussion Paper. |
AgenesisLack of cartilage (preterm)Low placement (chromosomal disorder, intellectual disability, kidney disorder)Preauricular tag or sinusSize: possibly overly prominent or protruding ears |